
NEWS > Everything you need to know about an Achilles tendon that hurts
Everything you need to know about an Achilles tendon that hurts
Posted by Raffaello Riccio in Achilleo, Foot Surgery, minimally invasive surgery, percutaneous surgery, Hollow foot, Flat foot, posture, prolotherapy, push up test, High heels, Tendinitis, Tendinosis, Uncategorized07 Mar2018
What is Achilles Tendinopathy?
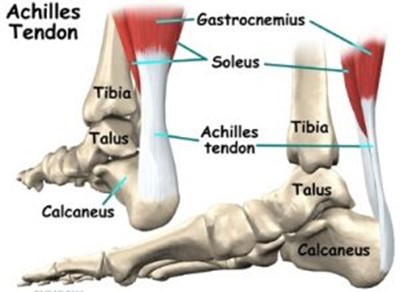
Achilles tendinopathy is a frequent condition of suffering of the Achilles tendon, a large tendon located in the back of the leg and ankle, and the cause of pain along the back of the leg, up to the heel.
The Achilles tendon is the largest tendon in our body, it connects the calf muscle to the heel bone, and is stressed when we walk, run, jump. Although it can withstand great stresses, during these activities the Achilles tendon is exposed to developing an often painful condition, which is often associated with trauma or its excessive or improper use.
SThere are two types of Achilles tendinopathy in relation to the affected area of the tendon:
Non-insertional Achilles tendinopathy
It affects the central part of the tendon, and is associated with an initial degeneration of the tendon itself with microlesions in its structure, swelling and tendon thickening. It is the most common type of tendinopathy in young and active patients.
Insertional Achilles tendinopathy
It affects the final part of the tendon, near its insertion on the calcaneus, and often also affects inactive patients and older years.
In both types of Tendinopathy, the affected tendon fibers can undergo calcifications; moreover bone spurs often appear in the insertional forms (calcaneal spines).
What is the difference between Tendinitis and Tendinosis?
Inflammatory suffering of the Achilles tendon is called Tendonitis, and must be distinguished from another common condition that can affect this tendon, this time of a degenerative type, called Tendinosis.
Patients with a tendinosis have chronic pain and swelling in the Achilles tendon, as a result of a degenerative process that is often associated with microlesions in its structure.
The nature of Tendinosis is not well understood. And unfortunately, many patients and doctors confuse the terms Tendinitis and Tendinosis.
Inflammation versus Degeneration
The term Tendonitis refers to inflammation of the Achilles tendon. Inflammation is most often an acute event (result of a sudden trauma); and is characterized by swelling, redness, warmth and pain. Under the microscope, the intervention of those cells that our body sends to the affected area in situations of inflammation is found to control the process and heal the affected tendon.
Achilles tendinosis, on the other hand, is a different condition, which is not characterized by inflammation. Therefore, there are no inflammatory symptoms such as redness and heat of the surrounding tissues; although the tendon may be painful to the touch, there is generally no acute pain, rather the prevailing sign is the degenerative thickening of the tendon itself.
Achilles tendinosis is a chronic problem, therefore it develops gradually and tends to persist over time. Under the microscope, there is an absence of inflammatory cells, although microlesions and degeneration of the tendon fibers are found.
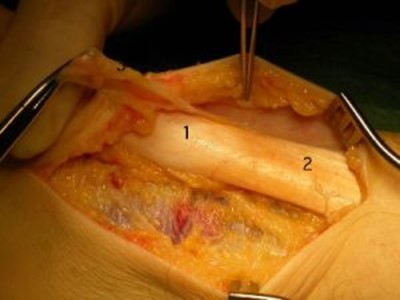
Appearance of a tendon sinew
What are the causes?
The causes of Achilles tendinopathy are not fully understood, although there is a relationship with a sudden increase in the intensity of physical activity performed. Tendinopathy can be associated with repetitive activities that produce functional overload on the tendon, postural imbalances associated with flat or pes cavus, inadequate footwear, and overly rigid training surfaces.
In any case, Achilles tendinopathy is typically not related to a specific trauma, but to repeated stresses over time on the tendon itself. This occurs especially when we push our body to do too much or too fast, but other factors can contribute to the development of this condition:
• A sudden increase in the amount or intensity of physical exercise; for example, the sudden increase in the training load without giving the body the opportunity to gradually get used to it.
• The retraction of the calf muscles; With a retraction of the calf muscles, an aggressive exercise program can put undue stress on the achilles tendon fibers.
• A bone spur (heel spur) if it appears when the tendon is inserted on the heel, it can irritate the tendon itself and cause pain.
What are the symptoms of Achilles tendinopathy?
Back pain in the ankle and lower leg is the main symptom, especially when the area between 2 and 4 cm above the insertion of the tendon on the heel is affected.
This part of the tendon normally receives a poor blood supply, making it particularly prone to developing a distressing condition.
Pain is typically more significant after periods of inactivity; therefore patients generally complain of pain in the first steps in the morning and when they get up after sitting for a long time. Naturally, pain will appear in physical activity, especially in running and jumping.
The most common symptoms include:
• Pain and stiffness in the morning
• Pain in the heel and tendon that worsens with physical activity
• Severe pain the day after physical exercise
• Thickening of the tendón
• Bone spur
• Swelling always present that gets worse throughout the day
Sometimes a sudden painful snap in the back of the calf appears on these symptoms; in these cases it is necessary to think of a possible rupture of the Achilles tendon.
How is the suspicion of Achilles tendinopathy confirmed?
The diagnosis of Tendinitis is essentially based on clinical examination. In any case, in the suspicion of Achilles tendonitis, diagnostic investigations should be performed:

Radiographic examination: highlights the bone structures well. It can show if calcifications have formed in the tendon. Calcifications upon insertion of the tendon indicate insertional tendinopathy. A calcification in the middle part of the tendon instead indicates a severe non-insertional tendinopathy (Tendinosis).
Ultrasound: Diagnostic examination that, in expert hands, can dynamically provide us with the best information on the condition of the tendon and surrounding soft tissues. Also very useful for guiding any infiltrative therapy in the tendon.
Magnetic resonance imaging (MRI): Although it is not a necessary investigation to diagnose tendonitis, it is important for planning surgery. MRI can show how severe the tendon damage is. If surgery is required, the surgeon will choose the most suitable technique based on the extent of the injury.
What are the options for conservative (non-surgical) treatment?
The best treatment for Achilles tendon problems is prevention. Achilles stretching exercises before physical activity, but also at the beginning of the day, will help maintain the elasticity and length of the posterior muscle chains, and the flexibility of the ankle.
Problems in the structure of the foot can be treated with orthoses inside the shoe. Orthotics and heel pads can be used to control overpronation of the hindfoot and prevent tendon pain.
Rest: The first step to reducing pain is to decrease or stop the activities that make it worse. For those who regularly engage in high-impact physical activity (such as running), it is advisable to switch to low-impact activities, which will place less stress on the Achilles tendon. Cross-training activities such as cycling and swimming are low impact activities that will help the patient stay active.
In severe cases, immobilization in braces may be necessary to allow the inflamed tissues to return to a normal condition more quickly. The duration of immobilization must, however, be limited as much as possible to avoid secondary phenomena of muscle stiffness or atrophy.
Prolotherapy is the technique I use for the treatment of tendinosis. It is a method that belongs to the chapter of Regenerative Orthopedic Medicine. It consists of an infiltrative therapy that uses “irritating” glucose solutions capable of stimulating a low-grade inflammatory response in the treated tendons, and a consequent series of events that lead, over a few weeks, to healing and regeneration of the damaged structure.

Although it is a relatively new and little known method in Italy (while it is on the contrary widespread and used in the United States), Prolotherapy is a very safe, very minimally invasive, not very painful technique, free of side effects, and which requires a small course of treatments, usually 2-3 sessions, to achieve healing.
In the same way that a fever makes us feel bad, but it is really an essential step in our process of healing from an infection in our body, so local inflammation causes transient pain but is our body’s healthy response to trauma, as it concentrates the factors necessary for healing in the area affected by the inflammatory process.
The term Prolotherapy broadly indicates the process of irritation of a tendon or ligament induced by the local injection of glucose, which has the purpose of stimulating its repair. The process is induced both by the mechanical stimulus (from the needle that pricks the tendon) and by the injected substance (glucose, PRP, or a combination of these).
The PRP (Platelet Growth Factors) which currently enjoys a certain appeal, is a method in which the patient’s blood is drawn and centrifuged before being injected into the suffering tendon, in order to concentrate the platelets and, presumably, increase their healing power. It is a painstaking and expensive technique, the results and advantages of which compared to Prolotherapy using glucose are not yet fully understood.
Cortisone injections: Cortisone is a powerful anti-inflammatory. Injections of cortisone into the Achilles tendon are not recommended as they can cause necrosis of the fibers and rupture of the tendon itself.
Shockwaves: High-energy shockwaves can stimulate the healing process in the damaged tendon. Representing a non-invasive and low-risk treatment, even if very painful, they can possibly be considered before planning surgery.
Anti-inflammatories (NSAIDs): They reduce pain and swelling, but not the thickening of the degenerated tendon; and of course they must be used with great caution.
In most cases, nonsurgical treatment will lead to healing and pain will subside, although it may take a few months for symptoms to disappear completely. Even with early treatment, symptoms can last longer than 3 months. If, on the other hand, the treatment is started several months after the onset of symptoms, it may take up to six months before this takes effect, with understandable damage and frustration for the most active and sporty patients.
What are the exercises that can help in Achilles tendinopathies?
The following exercises can help strengthen the calf muscles and reduce stress on the Achilles tendon.

Calf Stretch Bend forward against a wall with one knee extended and the heel on the ground. Place the other leg in front with the knee bent. To stretch the calf muscles and tendon, push the pelvis towards the wall in a gradual and controlled manner. Hold for 10 seconds and rest. Repeat the exercise twenty times on each side. A strong tension in the calf should be felt during the exercise.
Physiotherapy: It is very useful in the treatment of Achilles tendinopathies. It works better in Tendinosis than in Tendinitis.
Eccentric toning protocol: Eccentric toning is defined as the contraction of a muscle while it is stretching. It can cause damage to the Achilles tendon if it is not done correctly. It should initially be performed under the supervision of a physiotherapist. Only after having mastered the exercises is it possible to do them at home. These are exercises that can cause some discomfort that must not be unbearable:
EHeel Drop Exercises
Stay positioned on the edge of a step, with only the front of your foot on the step. This position will allow your heel to move up and down without hitting the step. Pay attention to balance yourself correctly to avoid falls or trauma. Keep your hands on a support to help balance. Bring your heels up and then slowly lower them to the lowest possible point. Repeat the exercise 20 times. The exercise must be done in a slow and controlled way. Moving too fast can risk damaging the tendon. As the pain improves, you can increase the difficulty of the exercise by holding a small weight in your hand.
What are the options for surgical treatment?
Surgical treatment should be considered for Achilles tendonitis only if the pain does not improve after 6 months of conservative treatment. The type of surgery depends on the location of the tendinopathy and the extent of the tendon damage.
Retraction of the gastrocnemius: it consists of a surgical lengthening of the calf muscle (gastrocnemius). Since a retracted calf muscle causes increased strain on the achilles tendon, this surgical procedure will be useful for patients who have difficulty dorsiflexing the foot despite an adequate stretching program.
In the retraction of the gastrocnemius, one of the two muscles that form the calf is stretched to improve the mobility of the ankle. The procedure can be performed with a traditional technique and incision or with a minimally invasive approach, which involves a mini incision and the aid of an endoscope, an instrument containing a small camera.
The frequency of complications for this type of surgery is low, but damage to a nerve branch can sometimes occur. The retreat of the gastrocnemius may or may not be associated with a debridement, which consists in the removal of damaged tendon tissue.

Debridement and Repair: (in cases where the tendon is damaged less than 50%) The goal of the surgery is to remove the damaged part of the tendon. Once this is removed, the remaining part of the tendon is repaired with plastic surgery, and sutures.
In insertional tendonitis, the heel spur must also be removed. The repair of the tendon in these cases may require the use of metal or plastic anchors to firmly secure the tendon fibers to the heel bone.
After this type of surgery, patients are allowed to walk in a brace for a period of between 2 and 4 weeks, depending on the extent of the tendon damage. An early passive mobilization, however, will be started already in the first days of the post-operative.
Debridement with tendon transposition: (when the tendon damage is greater than 50%) In these cases the still healthy part of the tendon is not strong enough for its proper functioning. To prevent its definitive rupture during activity, a tendon transposition is performed. The tendon that flexes the big toe (long flexor of the big toe) is transposed to the heel bone in order to reinforce the damaged and weakened Achilles tendon and improve its vascularization.
Despite the transposition surgery, the big toe will continue to move normally, and most patients will not feel any difference in walking or running. In relation to the extent of tendon damage, it is possible that, despite the surgery, some patients are unable to return to competitive physical activity.
What are the results of treating an Achilles tendinopathy?
Results: Most patients get good results from surgery. The main prognostic factor is the extent of the tendon damage.

The greater the damage, the longer the recovery time, and the less likely it will be to return to a sporting activity, especially if competitive.
Non-surgical treatment of Tendinitis takes several months but leads to healing and return to previous activities in 90% of cases. In patients in whom this treatment fails, surgery will be resolved between 75% and 100% of cases.
The results of Tendinosis treatment are less predictable. The successes of surgery in the various series range from 36% to 100%. The best results are associated with the shorter duration of symptoms, the lower degree of tendon damage, young age, and possible tendon transposition.
Physiotherapy plays an important role in the healing process. Many patients require 12 months or more of rehabilitation before being able to return to sports without pain.
